 Before I could explain my recent breast cancer diagnosis to Samantha, I had to understand it myself. How could this have happened? No one in my family has breast cancer. I was never a smoker or heavy drinker. I exercise, eat healthy and maintain my weight. I even take all of the vitamins recommended by my doctor.
Before I could explain my recent breast cancer diagnosis to Samantha, I had to understand it myself. How could this have happened? No one in my family has breast cancer. I was never a smoker or heavy drinker. I exercise, eat healthy and maintain my weight. I even take all of the vitamins recommended by my doctor.
Obviously, my yearly mammograms, sonograms and healthy lifestyle choices did not protect me, EXCEPT for discovering the cancer early. Am I really saying the “C” word?
“It’s malignant,” my doctor called with my biopsy results. “But don’t worry, you’ll be fine. It’s very small, only 9 millimeters, probably stage 1,” he tried to reassure me.
His voice was surreal. I felt like I was having an out of body experience, as though he was talking about someone else’s cancer and I happened to overhear it. I forced myself to breathe.
“You have the most common type, ductal carcinoma in situ,” he continued, “and ductal carcinoma aggressive…hormone positive… You’ll need a lumpectomy and targeted radiation and you’ll have to go off your hormone replacement. It will suck for a while but then it’ll be over. You’ll live. Don’t worry.”
I was terrified. “Do you promise?”“I haven’t lost a patient in 30 years,” he hedged. “And I have a wonderful surgeon who operated on my wife 16 years ago, and she’s created a lot of sculpture since then.”
I tried to breathe normally, but the air felt impossibly thick. “Can I call you later with my husband after I have some time to absorb this information? I know there are lots of questions I’m not asking.”
Many hours later I told Samantha, and she almost burst into tears. “How can you have breast cancer? Why?”
 “Bad luck.”
“Bad luck.”
“Are you going to be okay? “Can I still hug you?” Samantha threw her arms around me and held me in a vise-like grip. “I don’t want you to go away.”
“I’m not going anywhere.” I hugged her back. “I need to have surgery and radiation, but I’ll be okay.”
“What’s radiation?”
“Special light therapy targeted to make sure that there are no more cancer cells after the surgery. But first I need to heal.”
My daughter hugged me as if she would never let go. “Do you mind if I keep hugging you? I can’t help myself.”
I smiled and felt like crying at the same time. “I love your hugs. Just be gentle with my right side. It still hurts from the biopsy and that’s where my surgery will be.”
My life became a blur. My MRI and core biopsy were on Friday; the diagnosis was Monday afternoon. On Wednesday morning we met the surgeon and scheduled surgery for the following Thursday. I spent the afternoon before the lumpectomy having pre-surgical procedures: another MRI, injection of dye and seed placement and a lymph node biopsy. Every day I filled out seemingly endless on-line forms, forgot and reset my password multiple times and worried about pre-authorization
“You’re going to be fine,” the surgeon assured me as he entered the room. “I just want you to know that your hormone replacement therapy did not cause this cancer and nothing you did in your life made this happen,” as if answering Samantha’s question along with my own. “The good news is your radiologist caught it really early. Some radiologists would have missed it. You should send her a good bottle of wine.”
“What about recurrence?” I had to ask.
“You’re 95% plus plus plus safe to live a normal life.”
“Do you promise?”
“Yes.” His eyes were smiling above his mask. He patiently explained the pre-surgical procedures scheduled for the day before my lumpectomy.
 What a relief to put my life in the hands of a trusted surgeon who is both brilliant AND kind! A rarity in today’s frenetic and corrosively divided world. I was glad to have surgery scheduled as soon as possible. Only one more weekend to live with a tiny ticking time bomb in my chest. After that, I would only be holding my breath until Wednesday at 11:15 am. Three more days of waiting and then a week to recover.
What a relief to put my life in the hands of a trusted surgeon who is both brilliant AND kind! A rarity in today’s frenetic and corrosively divided world. I was glad to have surgery scheduled as soon as possible. Only one more weekend to live with a tiny ticking time bomb in my chest. After that, I would only be holding my breath until Wednesday at 11:15 am. Three more days of waiting and then a week to recover.
Each day after the diagnosis and before the surgery felt like forever. I was eager to get through the lumpectomy and sprint to the finish line with cancer forever defeated. But I remembered the advice from Samantha’s world-famous psychiatrist, Dr. Stanley Greenspan. Samantha was 14 months old, and had already been diagnosed with PDD when he offered me some guidance. I had impatiently waited two months for our first appointment with Dr. Greenspan and I was desperate to help Samantha overcome her challenges and catch up to her neurotypical twin brother as quickly as possible.
“Marguerite, you have to treat this journey as a marathon, not a sprint,” Dr. Greenspan warned. “Otherwise you’ll be too exhausted and stressed out to help your daughter.”
Sage advice, although often very difficult to follow. I had to learn to be patient through years of frustration and sadness, always hoping for faster progress and telling myself to enjoy small victories. Always remaining optimistic through the worst of times, yet always aware that more hurdles might lie ahead.
Now that my breast surgery is behind me, I’m recovering nicely. The surgeon assured us that everything went well and not to worry. That’s what I’ve told Samantha every day since the lumpectomy—along with a reminder to hug me gently. As a role model for my daughter, I’m trying to stay confident and pace myself for whatever treatment is recommended next.
I’m still waiting for lab results, so stay tuned.



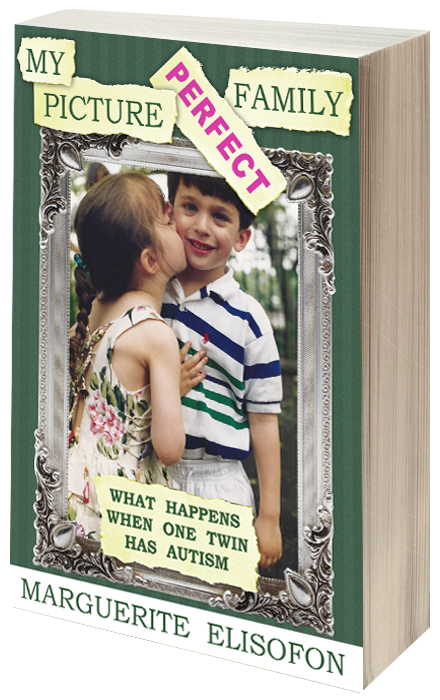

 Marguerite Elisofon is a New York City writer and the author of My Picture Perfect Family, a memoir about how her family navigated life with a child on the autistic spectrum before the internet and support groups existed. She also blogs about parenting young adults and disability related issues in The Never Empty Nest. Her writing has been featured in a variety of publications, including Time and NY Metro Parents magazine, and her family’s story has been featured by the NY Post, Fox News, The Daily Mail, and on Jenny McCarthy’s Dirty Sexy Funny radio show. A Vassar graduate, Marguerite was born and raised in New York City, where she still lives with her husband, Howard, in their mostly-empty nest. She is available to speak about a wide variety of issues relating to twins, parenting, and autism.
Marguerite Elisofon is a New York City writer and the author of My Picture Perfect Family, a memoir about how her family navigated life with a child on the autistic spectrum before the internet and support groups existed. She also blogs about parenting young adults and disability related issues in The Never Empty Nest. Her writing has been featured in a variety of publications, including Time and NY Metro Parents magazine, and her family’s story has been featured by the NY Post, Fox News, The Daily Mail, and on Jenny McCarthy’s Dirty Sexy Funny radio show. A Vassar graduate, Marguerite was born and raised in New York City, where she still lives with her husband, Howard, in their mostly-empty nest. She is available to speak about a wide variety of issues relating to twins, parenting, and autism. 
Fingers and toes crossed you get the right lab results. Love you!!!
Thanks. I did. So far, so good…
Thanks for sharing your path here, Marguerite. Samatha’s too. We carry you in our hearts.
I carry you and your daughters in my heart too.
Marguerite…wishing you good health and good hugs. May your connection with Samantha grow. Thank you for alerting us to the fickleness of life.
I carry you and your daughters in my heart too.